Whether they practice medicine in a rural or urban location, all doctors need to maintain their complex medical procedural skills, particularly for ones they may only perform infrequently, such as intubating infants and young children. .
Historically, such training has only been available in-person, and in larger urban centres. And travelling to receive training often means there is no one to look after their patients back home.
Ontario Tech University researcher and Canada Research Chair in Health Care Simulation Dr. Adam Dubrowski says that new simulation technology may have the potential to help doctors hone their skills in their own practice without leaving their patients unattended.
“Simulation means creating a situation or environment that lets learners safely practice skills, instead of doing it in real life,” says Dr. Dubrowski, a Professor with Ontario Tech’s Faculty of Health Sciences. “Through a research-based approach, we believe the simulators we’re designing can make a big difference in how rural and remote doctors learn and keep their life-saving skills up to date, without leaving their patients alone.”
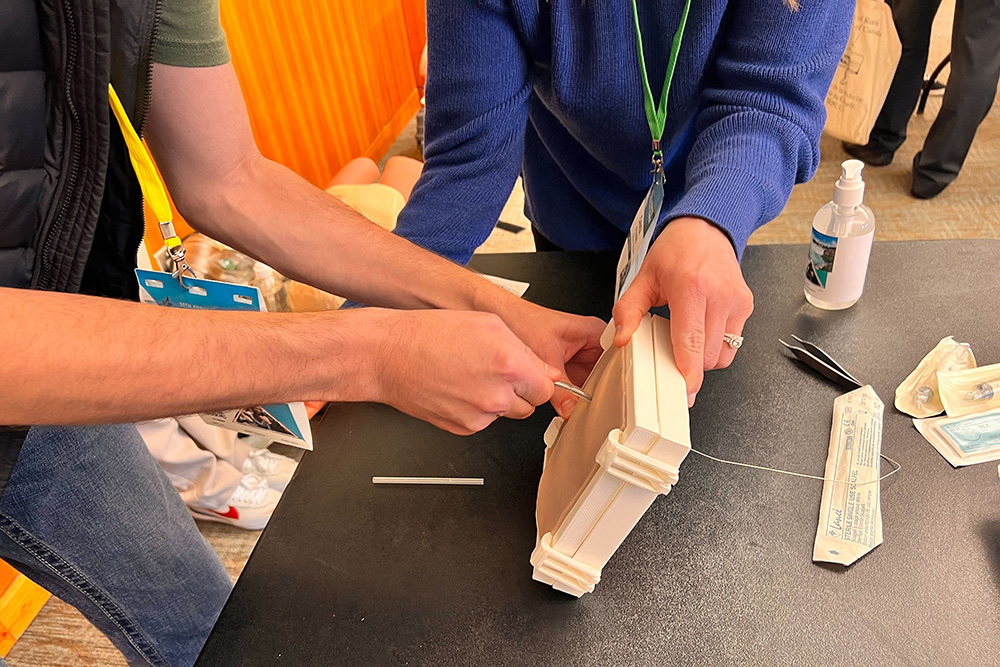
For the past few years, Dr. Dubrowski and his maxSIMhealth Laboratory at Ontario Tech have been collaborating with the Society for Rural Physicians of Canada (SRPC), which provides professional skills development workshops annually for all rural and remote physicians in Canada. In April 2023, an eight-person Ontario Tech team featuring the maxSIMstarters (an affiliated Faculty of Health Sciences undergraduate student-interest club) attended the SRPC’s 30th Annual Rural and Remote Medicine Course in Niagara Falls.
“With support from the Canadian Foundation for Innovation, our lab uses 3D printing and other advanced techniques to create special simulators,” explains Dr. Dubrowski. “The simulators that were made for SRPC were co-designed by maxSIMhealth together with health-care experts to be customizable, accurate, and affordable. In the last six months, our graduate students collaborated with the SRPC leaders and educators to make nine of these simulators. And then, our undergraduate students, the maxSIMstarters, helped build more than 300 individual units.”
The simulators were a huge hit at the SRPC event in Niagara Falls. The learning participants gave the units an average 4.4 out of 5 for how well they helped them learn, and 4 stars for how realistic they felt compared to traditional surgery simulations performed on animals .
“Our goal for 2024 is to make the simulators even better and aim for a 5-star rating at the event. Once we establish that these simulators are effective in the workshops the way they are currently ru, we will try to send them to the doctors to where they need them. The SRPC also mentioned that they want to help by creating an online learning system. This system is being developed by Dr. Bill Kapralos of Ontario Tech’s Faculty of Business and Information Technology (co-lead of maxSIMhealth Laboratory) and his graduate student Andri Torres.”
Advantages of simulation over historic training methods involving animals
In the past, the SRPC used animal parts like pigs' feet and chicken bones to simulate medical procedures. For example, they would use pigs' feet to practice stitching up skin and chicken bones to teach doctors how to give fluids and medicine through a patient's bone. They also used cow ribs to show how to treat a collapsed lung by puncturing the torso.
The previous use of animal-based simulators for training has some issues and limitations, including ethical concerns. Animals also have different bodies than humans, so the training may not be as accurate. Another drawback is simulations using animals can be expensive to get and take care of.
“Because of these reasons, more and more people are asking for different ways to train, like using affordable synthetic simulators that look like human bodies,” says Dr. Dubrowski. “These alternatives are better because they are ethical, precise, affordable and can be customized to specific needs.”
Media contact
Bryan Oliver
Communications and Marketing
Ontario Tech University
289.928.3653 (mobile)
bryan.oliver@ontariotechu.ca